A measles outbreak in the Columbus, Ohio, area has nearly tripled in the last two weeks as officials say they’re struggling to identify the geographic spread of the outbreak and expect it to drag on for months.
Confirmed cases have risen from 18 in mid-November to the confirmed case count of 50, as of Friday morning. Twenty of the cases have required hospitalization. No deaths have been reported.
All of the sickened children are entirely unvaccinated. Nine of the cases are in babies under the age of 1 year, who are typically not yet eligible for vaccination. Twenty-six cases are in infants ages 1 to 2 years—who are eligible for their first dose. Ten cases are in toddlers ages 3 to 5—some of whom would have been eligible for their second dose—and there are five cases in children between the ages of 6 and 17.
In a press conference earlier this week, health officials said that at least 25 percent of the area’s 2-year-olds have not been vaccinated with the safe and effective MMR vaccine, which protects against measles, mumps, and rubella. Based on census data from Franklin county, which encompasses Columbus, that means than tens of thousands of area children are vulnerable to the highly infectious virus that can easily turn severe and even life-threatening in young children.
Expected to grow
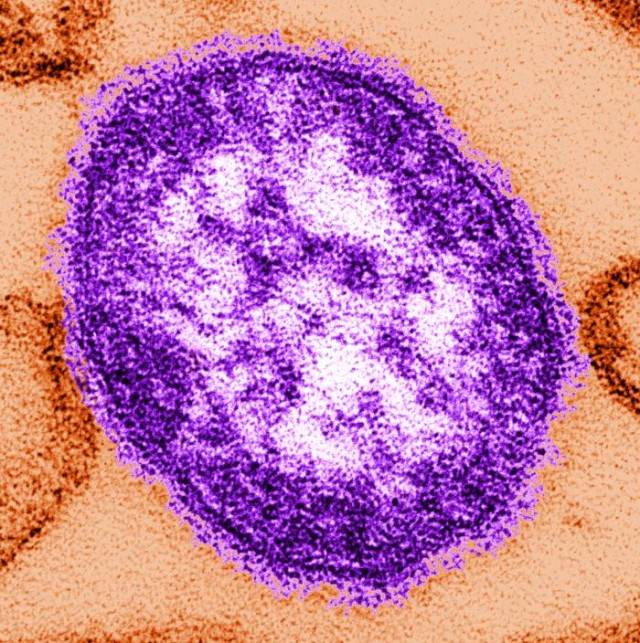
Measles is an airborne virus, spread via coughing, talking, or even being in the same vicinity as an infected person. In indoor spaces, the virus can linger in the air for up to two hours after an infected person has passed through. The Centers for Disease Control and Prevention estimates that up to 90 percent of unvaccinated people exposed to the virus will become infected.
“I do expect our numbers to continue to grow,” Mysheika Roberts, public health commissioner for Columbus, said in a press conference this week. “In talking to the CDC and our colleagues across the country who’ve experienced measles outbreaks, this can last several months.”
Local health officials are now working closely with the CDC and the Nationwide Children’s Hospital to address the cases and try to curb the outbreak. But, Roberts acknowledged in the press conference that they’re still having trouble getting a handle on the outbreak’s scope.
For instance, in some measles outbreak responses, health officials can make the decision to preemptively vaccinate infants ages 6 to 11 months old if they’re considered at high risk of infection—infants are typically eligible for their first MMR dose at 12 months, with a second dose given between the ages of 4 and 6. But, that early vaccination strategy is typically deployed when epidemiologists can pinpoint the communities at risk, which is not the case in Columbus.
“We have been in discussion with the CDC about that,” Roberts said. “Communities that have done that in the past have been able to really define the geographic location of where the cases are. We are not certain that we can really restrict the geographic area. So, we’re looking into that closely. We’re working with our colleagues at CDC [and] really trying to map out where these cases are to see if there is a segment of our community that we could offer that as an option to parents.”
Roberts noted that, so far, the outbreak spans three public health jurisdictions: Columbus Public Health, Franklin County Public Health, and the Ross County Health District. Ross County is about 47 miles south of Franklin county, with another county, Pickaway, in between the two.
“Get them vaccinated now”
In addition to the three geographic areas, Roberts also noted three specific locations where confirmed cases were known to have been contagious, which included a grocery store, a church, and a mall. She listed out the locations, dates, and times of potential exposures down to the hours, accounting for the possibility of the virus lingering for up to two hours.
“We have no way of informing individuals in those areas without going to the media,” Robert said.
The 50 cases so far are all counted from November 7 onward and are considered to be from local community spread of the virus. There were four other travel-related cases in the area earlier in the year, between June and October. It’s unclear how the current outbreak began, but officials suspect it is connected to one of the earlier travel-related cases.
Ohio’s current 2022 total of 54 measles cases accounts for the bulk of the country’s total cases. The CDC listed a total of 55 cases nationwide as of November 24. But case numbers are expected to grow in Ohio. And with the anti-vaccine sentiments that have taken hold and missed vaccinations during the pandemic, health experts in the US and worldwide are bracing for a fierce resurgence of the highly contagious virus.
Vaccination against measles is highly protective and the best weapon to fight the potentially deadly infection. Roberts pleaded with local parents of unvaccinated children to get their children vaccinated as soon as possible with the virus swirling around their community.
“I strongly encourage those parents to get those kids vaccinated—now. Don’t wait. Don’t wait until after the holiday. Get them vaccinated now,” Roberts said.
She added that local health officials had opened vaccination clinics in recent weeks but had not seen an uptick in children getting MMR vaccines.
